The cardiovascular system stands as one of the most remarkable engineering marvels within the human body, orchestrating the continuous circulation of blood to sustain life itself. This intricate network of heart, blood vessels, and blood works tirelessly, pumping approximately 2,000 gallons of blood daily through more than 60,000 miles of vessels. Every beat of your heart represents a precisely coordinated event that delivers oxygen and nutrients to trillions of cells while simultaneously removing metabolic waste products. Understanding how this vital system functions provides invaluable insight into maintaining optimal health and preventing cardiovascular disease, which remains the leading cause of death globally. The complexity of cardiovascular physiology encompasses everything from microscopic cellular processes to large-scale hemodynamic principles that govern blood flow throughout the body.
Cardiac anatomy and structural components of the cardiovascular system
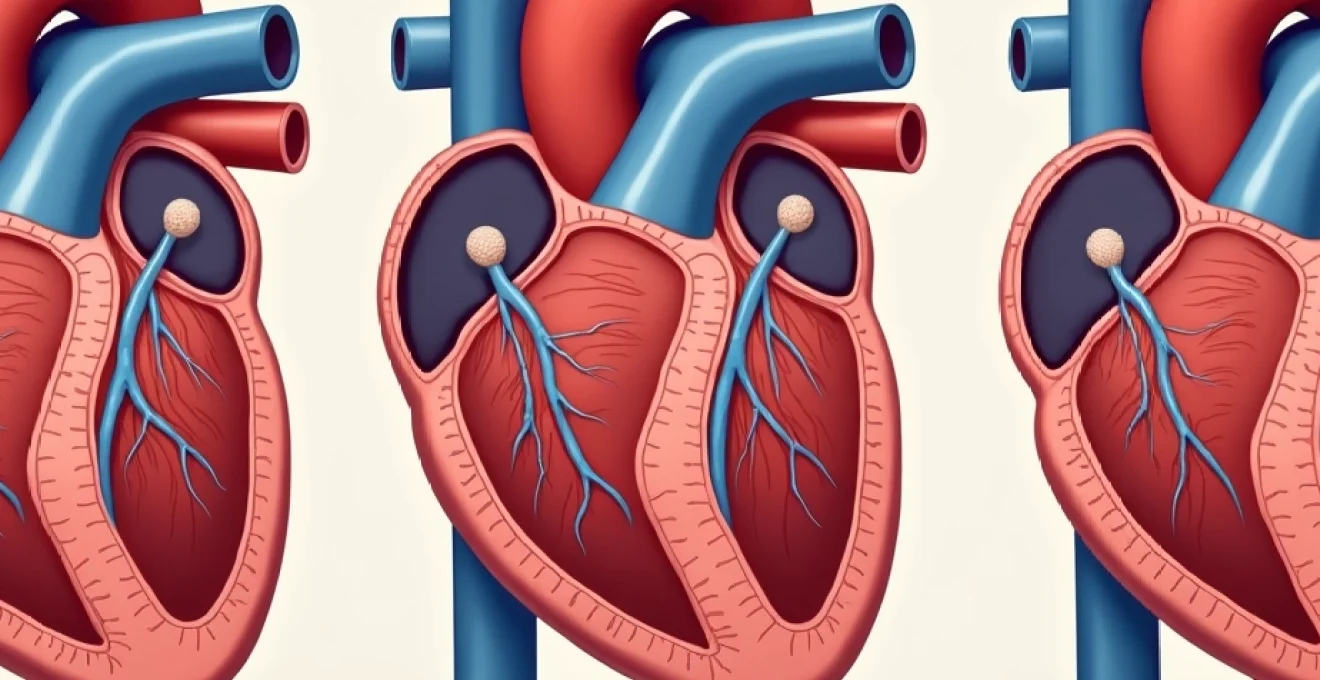
The human heart serves as the central pump of the cardiovascular system, positioned slightly left of centre within the mediastinal cavity of the thorax. This muscular organ weighs approximately 250-350 grams in adults and measures roughly the size of a closed fist. The heart’s strategic location allows it to function as a dual-sided pump, with the right side managing pulmonary circulation and the left side handling systemic circulation. The heart’s external surface is covered by the pericardium, a protective double-layered membrane that provides lubrication and prevents excessive cardiac motion during contraction.
Four-chamber heart architecture: atria and ventricular function
The heart’s internal architecture consists of four distinct chambers that work in synchronised pairs to maintain efficient blood circulation. The two atria serve as receiving chambers, with the right atrium collecting deoxygenated blood from the systemic circulation via the superior and inferior vena cavae, while the left atrium receives oxygenated blood from the pulmonary veins returning from the lungs. These thin-walled chambers act as temporary reservoirs, allowing blood to accumulate before being transferred to the ventricles below.
The ventricles represent the heart’s primary pumping chambers, featuring substantially thicker muscular walls compared to the atria. The right ventricle pumps blood through the pulmonary circulation at relatively low pressures, whilst the left ventricle generates the higher pressures necessary to drive blood throughout the entire systemic circulation. The interventricular septum separates these chambers, preventing the mixing of oxygenated and deoxygenated blood whilst contributing to the heart’s structural integrity.
Heart valve mechanisms: tricuspid, pulmonary, mitral, and aortic operations
Cardiac valves function as one-way gates, ensuring unidirectional blood flow through the heart’s chambers and into the great vessels. The tricuspid valve, located between the right atrium and right ventricle, consists of three leaflets anchored by chordae tendineae to papillary muscles within the ventricular wall. This arrangement prevents backflow during ventricular contraction whilst allowing efficient filling during diastole.
The mitral valve operates similarly between the left atrium and left ventricle but features only two leaflets, earning it the alternative name of bicuspid valve. The semilunar valves – pulmonary and aortic – guard the exits from the ventricles to their respective great vessels. These valves open during ventricular systole, allowing blood ejection, and snap shut during diastole to prevent regurgitation back into the ventricles.
Myocardial tissue composition and cardiac muscle fibre organisation
Cardiac muscle tissue exhibits unique characteristics that distinguish it from both skeletal and smooth muscle. The myocardium consists of interconnected cardiac myocytes linked by intercalated discs, which contain gap junctions and desmosomes. These specialised connections allow rapid electrical conduction and mechanical coupling between adjacent cells, enabling the heart to contract as a unified functional unit rather than individual muscle fibres.
The arrangement of cardiac muscle fibres follows a complex helical pattern that optimises the heart’s pumping efficiency. This three-dimensional organisation allows the ventricles to twist slightly during contraction, similar to wringing out a towel, which maximises the volume of blood ejected with each heartbeat. The endocardium lines the heart’s internal surfaces, providing a smooth interface for blood flow and housing specialised conduction system components.
Coronary circulation pathways: left and right coronary artery distribution
The coronary circulation supplies the heart muscle itself with oxygen and nutrients through a dedicated vascular network that branches directly from the ascending aorta. The left main coronary artery divides into the left anterior descending artery and the left circumflex artery, whilst the right coronary artery typically gives rise to the posterior descending artery and posterolateral branches. This distribution pattern ensures comprehensive perfusion of the myocardium, though individual anatomical variations are common.
Coronary blood flow exhibits unique characteristics, occurring primarily during diastole when the heart relaxes and intramyocardial pressures decrease. The coronary circulation can rapidly adapt to changing metabolic demands through autoregulation mechanisms, increasing flow during periods of increased cardiac work. Understanding coronary anatomy proves crucial for recognising how atherosclerotic disease can compromise myocardial perfusion and lead to ischaemic heart disease.
Vascular network design and blood vessel classification systems
The cardiovascular system’s vascular network represents a sophisticated distribution system that extends from large elastic arteries near the heart to microscopic capillaries within tissues, before collecting into progressively larger venous channels for return circulation. This hierarchical organisation optimises pressure gradients, flow velocities, and exchange functions according to the specific requirements of different vascular segments. The total cross-sectional area of the vascular system increases dramatically as blood moves from large arteries through capillaries, allowing for efficient nutrient and waste exchange at the cellular level.
Arterial structure and elastic recoil properties in major vessels
Large elastic arteries such as the aorta and pulmonary trunk feature walls composed of multiple layers of elastic fibres interspersed with smooth muscle cells and collagen. This composition allows these vessels to stretch during systole, storing energy like a compressed spring, then recoil during diastole to maintain forward pressure and flow. This Windkessel effect smooths the pulsatile output from the heart into more continuous flow in peripheral vessels.
As arteries branch and decrease in diameter, their walls contain proportionally more smooth muscle and less elastic tissue, transitioning into muscular arteries and eventually arterioles. These smaller vessels play crucial roles in regulating blood pressure and flow distribution through vasoconstriction and vasodilation. The ability of arterioles to change their diameter represents the primary mechanism for controlling peripheral resistance and, consequently, blood pressure.
Capillary bed architecture and microcirculation exchange mechanisms
Capillaries represent the functional units of the cardiovascular system where actual exchange between blood and tissues occurs. These microscopic vessels, measuring only 5-10 micrometers in diameter, have walls consisting of a single layer of endothelial cells surrounded by a basement membrane. This minimal barrier facilitates the diffusion of oxygen, nutrients, and waste products whilst preventing the loss of larger molecules such as proteins and blood cells.
Different tissues exhibit specialised capillary structures suited to their specific functions. Continuous capillaries in the brain maintain tight junctions forming the blood-brain barrier, whilst fenestrated capillaries in the kidneys and intestines allow for rapid filtration and absorption. Sinusoidal capillaries in the liver provide extensive surface area for metabolic processing and protein synthesis. The total surface area of all capillaries in the human body exceeds 600 square metres, highlighting the enormous capacity for molecular exchange.
Venous return systems and Valve-Assisted blood flow dynamics
The venous system faces the challenge of returning blood to the heart against gravity, particularly from the lower extremities. Venous return relies on multiple mechanisms including the skeletal muscle pump, respiratory pump, and the presence of one-way valves within veins. These valves prevent backflow and ensure that blood moves progressively towards the heart, even when venous pressures are low.
Venous compliance significantly exceeds arterial compliance, allowing veins to accommodate large volume changes with relatively small pressure changes. This property makes the venous system an important blood reservoir, containing approximately 70% of total blood volume at any given time. Venous return represents a critical determinant of cardiac output, as the heart can only pump the blood that returns to it.
Pulmonary circulation versus systemic circulation pressure differentials
The pulmonary circulation operates at significantly lower pressures than the systemic circulation, with typical pulmonary artery pressures of 25/10 mmHg compared to systemic arterial pressures of 120/80 mmHg. This pressure differential reflects the different functional requirements of each circulation: the pulmonary system prioritises efficient gas exchange over high-pressure perfusion, whilst the systemic circulation must overcome greater resistance to reach distant organs.
The lower pressure in pulmonary vessels reduces the workload on the right ventricle whilst maintaining adequate perfusion for gas exchange. Pulmonary vascular resistance can change dramatically in response to alveolar oxygen levels, a phenomenon known as hypoxic pulmonary vasoconstriction. This mechanism optimises ventilation-perfusion matching by redirecting blood flow away from poorly ventilated lung regions.
Cardiac electrophysiology and conduction system pathways
The heart’s electrical system generates and coordinates the impulses necessary for rhythmic contraction, operating independently of nervous system control through intrinsic pacemaker cells and specialised conduction pathways. This electrical activity originates from spontaneous depolarisation of specific cardiac cells, creating action potentials that spread throughout the myocardium in a precisely timed sequence. The cardiac conduction system ensures that atrial contraction precedes ventricular contraction, optimising ventricular filling and cardiac output. Understanding cardiac electrophysiology becomes essential for recognising how arrhythmias develop and how various interventions can restore normal heart rhythm.
Sinoatrial node pacemaker function and intrinsic heart rate control
The sinoatrial (SA) node, located in the right atrial wall near the entrance of the superior vena cava, serves as the heart’s primary pacemaker due to its fastest intrinsic firing rate. SA node cells exhibit automaticity, spontaneously depolarising approximately 60-100 times per minute through the gradual influx of sodium and calcium ions during phase 4 of their action potential. This pacemaker potential reaches threshold and triggers the next heartbeat without external stimulation.
The SA node’s firing rate responds to autonomic nervous system input, with sympathetic stimulation increasing heart rate through norepinephrine and epinephrine effects on calcium channels, whilst parasympathetic activity decreases heart rate through acetylcholine’s influence on potassium channels. Various factors including electrolyte imbalances, medications, and disease states can alter SA node function, leading to bradycardia or tachycardia.
Atrioventricular node delay mechanisms and bundle of his conduction
The atrioventricular (AV) node provides the only normal electrical connection between the atria and ventricles, located within the interatrial septum near the tricuspid valve. This specialised tissue introduces a deliberate delay of approximately 0.1-0.2 seconds in electrical conduction, allowing complete atrial emptying before ventricular contraction begins. The AV node’s slow conduction properties also protect the ventricles from excessively rapid atrial rhythms.
Following the AV node, electrical impulses travel through the Bundle of His, which penetrates the fibrous skeleton of the heart and divides into right and left bundle branches. These structures rapidly conduct impulses down the interventricular septum, ensuring coordinated ventricular activation. The bundle branches exhibit different conduction properties, with the left bundle further subdividing into anterior and posterior fascicles to optimise left ventricular electrical activation.
Purkinje fibre network distribution and ventricular depolarisation
The Purkinje fibre system represents the terminal portion of the cardiac conduction network, spreading throughout the ventricular walls to ensure rapid and coordinated muscle activation. These specialised fibres conduct electrical impulses at velocities exceeding 4 metres per second, allowing near-simultaneous depolarisation of ventricular myocytes. The Purkinje system’s extensive branching pattern ensures that electrical activation proceeds from the endocardium outward to the epicardium.
Purkinje fibres possess larger diameters and fewer gap junctions than ordinary cardiac myocytes, contributing to their rapid conduction properties. These cells also exhibit automaticity, though at slower rates than the SA node, providing backup pacemaker function if higher-level pacemakers fail. The distribution of Purkinje fibres varies between individuals, contributing to normal variations in electrocardiographic patterns.
Action potential phases and Calcium-Mediated contraction coupling
Cardiac action potentials differ significantly from those in nerve cells, exhibiting a characteristic plateau phase that prolongs depolarisation and prevents tetanic contractions. The action potential consists of five distinct phases: rapid depolarisation (phase 0), early repolarisation (phase 1), plateau (phase 2), repolarisation (phase 3), and resting potential (phase 4). Each phase involves specific ion channels and transporters that carefully control the electrical and mechanical events of the cardiac cycle.
The plateau phase, mediated primarily by L-type calcium channels, triggers calcium-induced calcium release from the sarcoplasmic reticulum, initiating muscle contraction through the interaction of actin and myosin filaments. This excitation-contraction coupling mechanism ensures that electrical activation reliably produces mechanical work. The prolonged refractory period associated with cardiac action potentials prevents premature contractions and maintains the heart’s rhythmic pumping function.
Haemodynamic principles and blood pressure regulation mechanisms
Haemodynamics encompasses the physical principles governing blood flow through the cardiovascular system, incorporating factors such as pressure, flow, resistance, and compliance. Blood pressure represents the force exerted by circulating blood against vessel walls, generated by cardiac output and modulated by peripheral vascular resistance. The regulation of blood pressure involves complex interactions between the heart, blood vessels, kidneys, and nervous system, maintaining adequate tissue perfusion whilst preventing damage from excessive pressures. Understanding haemodynamic principles proves essential for recognising how cardiovascular diseases develop and how therapeutic interventions can restore normal circulation. Poiseuille’s law demonstrates that flow through vessels depends on pressure gradients, vessel radius, blood viscosity, and vessel length, with vessel radius having the most dramatic impact on flow rates.
Blood pressure regulation operates through multiple time scales, from immediate baroreceptor responses to long-term hormonal adjustments involving the renin-angiotensin-aldosterone system. Short-term regulation primarily involves baroreceptors located in the carotid sinuses and aortic arch, which detect pressure changes and trigger rapid adjustments in heart rate and vascular tone through autonomic nervous system pathways. These mechanisms can restore blood pressure within seconds of a disturbance, such as standing up quickly or experiencing emotional stress. Long-term blood pressure control relies heavily on kidney function and fluid balance, as the kidneys adjust sodium excretion and blood volume in response to pressure changes.
The relationship between cardiac output and peripheral resistance fundamentally determines arterial blood pressure, making these two factors the primary targets for antihypertensive therapies.
Vascular autoregulation allows tissues to maintain relatively constant blood flow despite fluctuations in perfusion pressure. This mechanism operates through metabolic and myogenic responses, with arterioles constricting when pressure increases and dilating when pressure decreases. Metabolic autoregulation responds to local concentrations of oxygen, carbon dioxide, and metabolic byproducts, whilst myogenic autoregulation involves the intrinsic response of smooth muscle to stretch. These mechanisms ensure that vital organs receive adequate perfusion even when systemic blood pressure varies within reasonable limits.
Cardiovascular disease prevention and Long-Term health outcomes
Cardiovascular disease prevention strategies focus on modifiable risk factors that contribute to atherosclerosis and other pathological processes affecting the heart and blood vessels. Primary prevention targets individuals without established cardiovascular disease, emphasising lifestyle modifications and risk factor management to prevent disease development. Secondary prevention applies to those with existing cardiovascular conditions, aiming to prevent progression and reduce the likelihood of cardiovascular events such as heart attacks and strokes. The effectiveness of prevention strategies depends largely on early identification of risk factors and sustained implementation of evidence-based interventions throughout an individual’s lifetime.
Hypertension affects approximately one-third of adults globally and represents one of the most significant modifiable risk factors for cardiovascular disease. Blood pressure control through lifestyle
modifications and pharmacological interventions has proven remarkably effective in reducing cardiovascular morbidity and mortality. The Systolic Blood Pressure Intervention Trial (SPRINT) demonstrated that intensive blood pressure targets below 120 mmHg systolic significantly reduce cardiovascular events compared to standard targets below 140 mmHg. However, achieving these targets requires comprehensive approaches combining dietary sodium reduction, weight management, regular physical activity, and often multiple antihypertensive medications working through different mechanisms.
Dyslipidaemia management forms another cornerstone of cardiovascular disease prevention, with elevated low-density lipoprotein (LDL) cholesterol directly contributing to atherosclerotic plaque formation. Statin therapy has revolutionised cardiovascular prevention by reducing LDL cholesterol and providing additional anti-inflammatory benefits that stabilise atherosclerotic plaques. Recent guidelines emphasise achieving specific LDL cholesterol targets rather than simply prescribing standard doses, with some high-risk patients benefiting from LDL levels below 55 mg/dL. The addition of ezetimibe and PCSK9 inhibitors provides options for patients who cannot achieve targets with statins alone or experience statin intolerance.
Smoking cessation represents perhaps the most cost-effective cardiovascular intervention, with benefits beginning within hours of quitting and continuing to accumulate over years. Tobacco use accelerates atherosclerosis through multiple mechanisms including endothelial dysfunction, increased platelet aggregation, and promotion of inflammatory processes. The cardiovascular benefits of smoking cessation are substantial even for long-term smokers, with the risk of coronary heart disease dropping by 50% within one year of quitting. Modern smoking cessation programs combine behavioural counselling with pharmacological support through nicotine replacement therapy, varenicline, or bupropion, achieving success rates of 20-30% in motivated individuals.
Diabetes management requires particular attention due to the accelerated atherosclerosis associated with chronic hyperglycaemia. Glycaemic control through lifestyle modifications and medications not only prevents microvascular complications but also reduces macrovascular events when combined with aggressive management of blood pressure and cholesterol. Recent cardiovascular outcome trials have identified specific antidiabetic medications, particularly sodium-glucose cotransporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, that provide cardiovascular benefits beyond glucose control. These medications demonstrate particular efficacy in reducing heart failure hospitalisations and cardiovascular deaths in patients with established cardiovascular disease.
Exercise physiology and cardiovascular adaptation responses
Regular physical activity induces profound adaptations within the cardiovascular system that enhance both performance capacity and long-term health outcomes. These adaptations occur at multiple levels, from cellular mitochondrial changes to systemic improvements in cardiac output and vascular function. The cardiovascular benefits of exercise extend far beyond simple fitness improvements, encompassing protective effects against atherosclerosis, improved endothelial function, and enhanced autonomic balance that collectively reduce cardiovascular disease risk by 30-40% in active individuals compared to sedentary populations.
Cardiac adaptations to exercise training include both structural and functional changes that improve the heart’s pumping efficiency. Endurance training typically increases left ventricular chamber size and wall thickness, a phenomenon known as athlete’s heart, which allows for greater stroke volume and cardiac output during exercise. The resting heart rate decreases as stroke volume increases, reflecting improved cardiac efficiency through enhanced parasympathetic tone and reduced sympathetic activity. These adaptations allow trained individuals to achieve higher maximum heart rates and sustain elevated cardiac outputs during prolonged exercise without experiencing premature fatigue.
Vascular adaptations represent equally important responses to regular exercise, with improvements in endothelial function serving as a key mechanism for cardiovascular protection. Exercise training increases nitric oxide bioavailability, improving vasodilation and reducing arterial stiffness throughout the vascular system. The formation of new capillaries, termed angiogenesis, increases the surface area available for oxygen and nutrient exchange whilst providing alternative pathways for blood flow. These vascular adaptations contribute to lower blood pressure, improved insulin sensitivity, and enhanced oxygen delivery to working muscles.
The metabolic benefits of exercise training extend beyond immediate cardiovascular improvements to include long-term protective effects against metabolic syndrome and type 2 diabetes. Regular physical activity improves insulin sensitivity, reduces abdominal adiposity, and favourably alters lipid profiles by increasing high-density lipoprotein (HDL) cholesterol whilst reducing triglycerides. These metabolic improvements work synergistically with direct cardiovascular adaptations to provide comprehensive protection against atherosclerotic disease. How can sedentary individuals safely transition to more active lifestyles whilst maximising cardiovascular benefits?
Exercise prescription for cardiovascular health should follow evidence-based guidelines that specify frequency, intensity, time, and type of physical activity. The current recommendations suggest at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, combined with muscle-strengthening activities on two or more days. However, even modest increases in physical activity provide significant cardiovascular benefits, with the greatest relative risk reduction occurring when completely sedentary individuals begin regular exercise programs. High-intensity interval training (HIIT) has emerged as a time-efficient alternative that produces similar or superior cardiovascular adaptations compared to traditional moderate-intensity continuous training.
The dose-response relationship between physical activity and cardiovascular health demonstrates that some exercise is good, more is generally better, but the law of diminishing returns applies at very high training volumes.
Special considerations apply when prescribing exercise for individuals with existing cardiovascular conditions, requiring careful assessment of exercise capacity and appropriate monitoring during initial training phases. Cardiac rehabilitation programs provide structured, medically supervised exercise training for patients recovering from heart attacks, cardiac surgery, or other cardiovascular events. These programs consistently demonstrate improved functional capacity, reduced symptoms, and decreased cardiovascular mortality when combined with comprehensive risk factor modification and patient education. The safety profile of supervised exercise training remains excellent even in high-risk populations, with serious adverse events occurring in fewer than 1 in 60,000 exercise sessions.
The psychological and neurological benefits of regular exercise contribute additional layers of cardiovascular protection through stress reduction and improved mental health. Physical activity stimulates the release of endorphins and other neurotransmitters that improve mood and reduce anxiety, whilst also providing a healthy outlet for managing life stresses that might otherwise contribute to cardiovascular disease risk. The social aspects of group exercise activities provide additional psychological benefits that enhance long-term adherence to active lifestyles. Understanding these multifaceted benefits helps explain why exercise remains one of the most powerful interventions for both preventing and managing cardiovascular disease across all age groups and risk categories.