The liver stands as one of the most resilient yet vulnerable organs in the human body, performing over 500 essential functions while silently processing everything from nutrients to toxins. Despite its remarkable regenerative capacity, liver disease affects approximately 4.5 million adults in the United States alone, causing around 57,000 deaths annually. What makes liver disease particularly insidious is its ability to progress silently for years, often remaining undetected until significant damage has already occurred. Understanding the early warning signs, diagnostic markers, and natural protective strategies can mean the difference between reversible liver damage and irreversible cirrhosis. Modern medicine offers sophisticated tools for early detection, while evidence-based natural interventions provide powerful support for hepatic health and regeneration.
Early clinical manifestations and biochemical markers of hepatic dysfunction
The liver’s remarkable ability to compensate for damage often masks early disease progression, making biochemical markers crucial for early detection. Most liver conditions remain asymptomatic until approximately 75% of liver function is compromised. However, subtle clinical manifestations and laboratory abnormalities can provide valuable early warning signals when properly interpreted within the clinical context.
Elevated serum aminotransferases: ALT and AST interpretation guidelines
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) serve as primary indicators of hepatocellular injury, though their interpretation requires careful consideration of various factors. ALT demonstrates greater liver specificity, as it is predominantly found in hepatocytes, while AST is present in multiple tissues including heart, muscle, and kidneys. Normal ALT ranges typically fall between 7-40 U/L for men and 7-35 U/L for women, though these values can vary between laboratories.
The pattern of aminotransferase elevation often provides diagnostic clues. An AST to ALT ratio greater than 2:1 strongly suggests alcoholic liver disease, particularly when accompanied by elevated gamma-glutamyl transferase levels. Conversely, viral hepatitis typically presents with ALT elevations exceeding AST levels. Massive aminotransferase elevations above 1000 U/L usually indicate acute hepatocellular necrosis from causes such as acetaminophen toxicity, viral hepatitis, or ischaemic hepatitis.
Bilirubin metabolism disruption and jaundice progression patterns
Bilirubin metabolism involves complex conjugation and excretion processes that become disrupted in liver disease. Total bilirubin levels above 2.5 mg/dL typically result in clinically apparent jaundice, first visible in the sclera before progressing to skin discolouration. The pattern of bilirubin elevation—conjugated versus unconjugated—provides crucial diagnostic information about the underlying pathophysiology.
Unconjugated hyperbilirubinaemia suggests haemolysis or inherited disorders like Gilbert’s syndrome, whilst conjugated hyperbilirubinaemia indicates hepatocellular dysfunction or biliary obstruction. Progressive jaundice accompanied by pale stools and dark urine suggests biliary obstruction requiring urgent evaluation. Fluctuating jaundice levels may indicate intermittent biliary obstruction or resolving acute hepatitis.
Alkaline phosphatase and Gamma-Glutamyl transferase elevation significance
Alkaline phosphatase (ALP) elevation indicates biliary obstruction or infiltrative liver disease, though it requires correlation with other markers for accurate interpretation. ALP is present in liver, bone, intestine, and placenta, necessitating fractionation or concurrent gamma-glutamyl transferase (GGT) measurement to confirm hepatic origin. GGT demonstrates high sensitivity for biliary disease and serves as an excellent marker for alcohol-related liver injury.
Combined ALP and GGT elevation strongly suggests cholestatic liver disease, whether from primary biliary cholangitis, primary sclerosing cholangitis, or drug-induced cholestasis. Isolated GGT elevation often indicates alcohol consumption or medication effects, particularly from phenytoin, barbiturates, or warfarin. The magnitude of ALP elevation helps differentiate between hepatocellular and cholestatic patterns of injury.
Prothrombin time prolongation and coagulation factor deficiencies
The liver synthesises most coagulation factors, making prothrombin time (PT) and international normalised ratio (INR) sensitive markers of hepatic synthetic function. Unlike other liver function tests, coagulation parameters reflect the liver’s biosynthetic capacity rather than cellular injury. PT prolongation indicates decreased synthesis of factors II, VII, IX, and X, with factor VII having the shortest half-life of approximately 6 hours.
Progressive PT prolongation suggests worsening liver function and carries prognostic significance in acute liver failure. An INR above 1.5 without anticoagulant therapy indicates significant hepatic dysfunction. However, vitamin K deficiency from malabsorption or poor nutrition can also prolong PT, requiring vitamin K administration to differentiate between nutritional and synthetic causes.
Differential diagnosis of major hepatic pathologies and risk factors
Accurate diagnosis of liver disease requires systematic evaluation of clinical presentation, laboratory findings, imaging studies, and risk factor assessment. Each major category of liver disease presents distinct patterns of biochemical abnormalities and clinical features that guide diagnostic workup and treatment strategies. Understanding these patterns enables clinicians to prioritise appropriate investigations and initiate timely interventions.
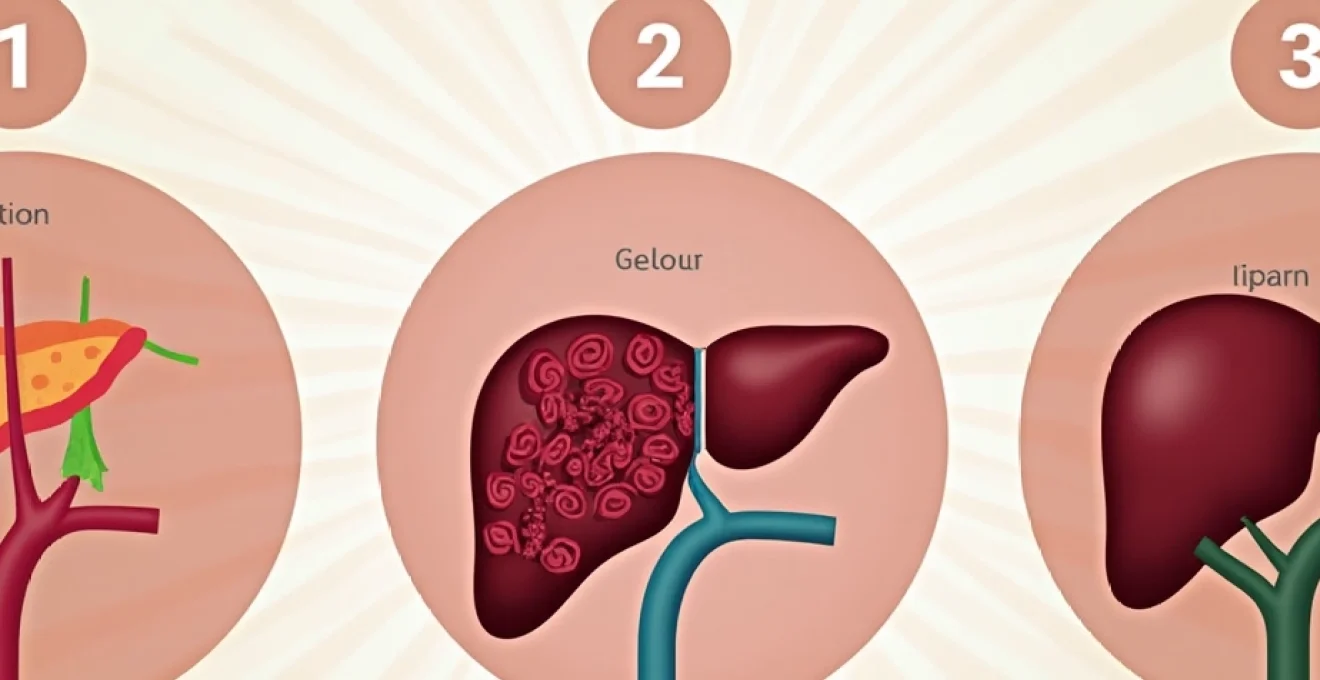
Non-alcoholic fatty liver disease spectrum: NAFLD to NASH progression
Non-alcoholic fatty liver disease (NAFLD), recently renamed metabolic dysfunction-associated steatotic liver disease (MASLD), represents the most common liver condition globally, affecting up to 25% of the population. NAFLD encompasses a spectrum from simple steatosis to non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and hepatocellular carcinoma. The condition closely associates with metabolic syndrome, type 2 diabetes, obesity, and dyslipidaemia.
NAFLD typically presents with mild aminotransferase elevation, often with AST to ALT ratios less than 1:1. Advanced fibrosis may develop silently, emphasising the importance of non-invasive fibrosis assessment. Risk stratification tools such as the NAFLD fibrosis score and FIB-4 index help identify patients requiring further evaluation. Lifestyle modification remains the cornerstone of treatment, with weight loss of 7-10% shown to reduce steatosis and inflammation significantly.
Viral hepatitis classification: hepatitis A, B, C, D, and E characteristics
Viral hepatitis encompasses five distinct viruses with different transmission routes, clinical courses, and long-term implications. Hepatitis A and E cause acute, self-limiting infections transmitted through the faecal-oral route, whilst hepatitis B, C, and D can establish chronic infections with potential for progressive liver disease. Understanding these distinctions guides appropriate testing, treatment, and prevention strategies.
Hepatitis B affects approximately 296 million people worldwide and can cause fulminant hepatic failure, chronic hepatitis, cirrhosis, and hepatocellular carcinoma. Hepatitis C, affecting 71 million globally, represents the leading indication for liver transplantation in developed countries. Direct-acting antiviral therapy now achieves sustained virological response rates exceeding 95% for hepatitis C, whilst hepatitis B requires lifelong antiviral suppression in most cases.
Alcoholic liver disease stages: steatosis to cirrhosis development
Alcoholic liver disease progresses through predictable stages, from fatty infiltration through alcoholic hepatitis to cirrhosis. The progression rate varies significantly based on genetic factors, gender, concurrent infections, and drinking patterns. Women develop alcoholic liver disease at lower alcohol consumption levels and progress more rapidly than men, possibly due to differences in alcohol metabolism and body composition.
Alcoholic steatosis represents the earliest and most reversible stage, occurring in virtually all individuals consuming more than 60g of alcohol daily. Alcoholic hepatitis may develop suddenly, presenting with jaundice, fever, and right upper quadrant pain. Severe alcoholic hepatitis carries significant mortality risk, with discriminant function scores helping stratify patients for corticosteroid therapy. Complete alcohol cessation remains essential for preventing disease progression and enabling potential reversal of early-stage disease.
Autoimmune hepatitis and primary biliary cholangitis diagnostic criteria
Autoimmune liver diseases result from immune system dysfunction targeting liver cells or bile ducts. Autoimmune hepatitis predominantly affects women and presents with elevated aminotransferases, hypergammaglobulinaemia, and circulating autoantibodies. Type 1 autoimmune hepatitis involves anti-nuclear antibodies (ANA) and anti-smooth muscle antibodies (ASMA), whilst type 2 disease involves anti-liver kidney microsomal antibodies (anti-LKM1).
Primary biliary cholangitis (PBC) targets intrahepatic bile ducts, causing progressive cholestasis and eventual cirrhosis. The condition demonstrates strong association with anti-mitochondrial antibodies, present in over 95% of cases. Early diagnosis enables treatment with ursodeoxycholic acid, which slows disease progression and improves transplant-free survival. Overlapping syndromes combining features of autoimmune hepatitis and PBC require complex treatment approaches addressing both inflammatory and cholestatic components.
Advanced diagnostic imaging and laboratory assessment techniques
Modern hepatology employs sophisticated diagnostic modalities that provide detailed assessment of liver structure, function, and fibrosis without invasive procedures. These techniques have revolutionised liver disease management by enabling early detection, accurate staging, and monitoring of treatment response. The integration of imaging biomarkers with clinical assessment enhances diagnostic precision whilst reducing patient discomfort and procedural risks associated with traditional liver biopsy.
Fibroscan elastography for Non-Invasive fibrosis staging
Transient elastography, commonly known as FibroScan, measures liver stiffness as a surrogate marker for fibrosis severity. The technique uses controlled attenuation parameter (CAP) to quantify hepatic steatosis whilst simultaneously measuring liver stiffness in kilopascals (kPa). Normal liver stiffness typically ranges from 2.5-7.0 kPa, with values above 12.5 kPa suggesting significant fibrosis requiring specialist evaluation.
FibroScan demonstrates excellent reproducibility and strong correlation with histological fibrosis stages across various liver diseases. However, interpretation requires consideration of factors that may affect measurements, including obesity, ascites, acute inflammation, and operator experience. Reliability criteria include achieving at least 10 valid measurements with an interquartile range to median ratio below 30%. The technique provides immediate results, enabling point-of-care decision-making and patient counselling.
Magnetic resonance elastography protocol for hepatic stiffness measurement
Magnetic resonance elastography (MRE) represents the most accurate non-invasive method for assessing liver fibrosis, demonstrating superior performance to transient elastography in challenging patient populations. MRE generates mechanical waves within liver tissue and maps the resulting displacement patterns to calculate tissue stiffness across the entire liver volume. This three-dimensional assessment provides more comprehensive fibrosis evaluation than point-measurements obtained with transient elastography.
MRE protocols typically employ 60 Hz mechanical waves delivered through a passive driver placed against the right chest wall. The technique demonstrates excellent accuracy for detecting advanced fibrosis (AUROC 0.92-0.96) and remains reliable in patients with ascites, obesity, or narrow intercostal spaces. Magnetic resonance imaging-proton density fat fraction (MRI-PDFF) can be performed simultaneously to quantify hepatic steatosis with exceptional precision.
Alpha-fetoprotein and PIVKA-II tumour marker analysis
Hepatocellular carcinoma surveillance relies on biomarker monitoring combined with imaging studies, particularly in high-risk populations with cirrhosis or chronic viral hepatitis. Alpha-fetoprotein (AFP) remains the most widely used biomarker despite limitations in sensitivity and specificity. AFP levels above 20 ng/mL warrant investigation, though benign conditions including active hepatitis and liver regeneration can cause elevation.
Protein induced by vitamin K absence or antagonist-II (PIVKA-II), also known as des-gamma-carboxy prothrombin, offers complementary diagnostic information to AFP. PIVKA-II demonstrates particular utility in detecting smaller tumours and monitoring treatment response. Combined AFP and PIVKA-II measurement improves diagnostic accuracy compared to either marker alone. Novel biomarkers including AFP-L3 fraction and circulating tumour DNA show promise for enhancing early detection capabilities.
Liver biopsy histopathological interpretation standards
Despite advances in non-invasive assessment, liver biopsy remains the gold standard for definitive diagnosis in selected cases, particularly when multiple disease processes are suspected or treatment decisions require precise histological characterisation. Modern biopsy interpretation employs standardised scoring systems that provide semi-quantitative assessment of inflammation, fibrosis, and specific disease features.
The METAVIR scoring system grades inflammation (A0-A3) and stages fibrosis (F0-F4), whilst the Ishak system provides more granular fibrosis assessment using a six-point scale. Adequate biopsy specimens require at least 20mm length with 11 or more portal tracts for reliable interpretation. Sampling variability remains a significant limitation, with studies demonstrating up to 25% discordance in fibrosis staging between different biopsy sites within the same liver.
Evidence-based hepatoprotective nutritional interventions
Natural hepatoprotective compounds offer promising adjunctive therapeutic options supported by emerging scientific evidence. These interventions work through various mechanisms including antioxidant activity, anti-inflammatory effects, and enhancement of cellular repair processes. While not replacing conventional medical therapy, evidence-based natural approaches can provide valuable support for liver health when integrated into comprehensive treatment plans under appropriate medical supervision.
Silymarin and milk thistle extract therapeutic mechanisms
Silymarin, the active compound complex derived from milk thistle (Silybum marianum), represents one of the most extensively studied hepatoprotective natural substances. The compound demonstrates multiple therapeutic mechanisms including antioxidant activity, anti-inflammatory effects, antifibrotic properties, and hepatocyte membrane stabilisation. Silymarin’s flavonoid components—silybin, silydianin, and silychristin—exhibit synergistic effects that protect against various hepatotoxic insults.
Clinical studies suggest silymarin may benefit patients with alcoholic liver disease, non-alcoholic fatty liver disease, and viral hepatitis, though results remain mixed. A systematic review of randomised controlled trials found modest improvements in aminotransferase levels but limited evidence for mortality benefit. Bioavailability represents a significant challenge , with standard preparations showing poor absorption requiring higher doses or pharmaceutical formulations with enhanced bioavailability such as phosphatidylcholine complexes or nanoparticle preparations.
N-acetylcysteine antioxidant pathway restoration
N-acetylcysteine (NAC) serves as a precursor to glutathione, the body’s primary intracellular antioxidant and critical component of hepatic detoxification pathways. NAC supplementation helps restore depleted glutathione stores in liver disease whilst providing direct antioxidant effects and supporting cellular repair mechanisms. The compound demonstrates particular efficacy in acetaminophen toxicity, where it serves as standard antidotal therapy.
Beyond acetaminophen poisoning, NAC shows promise in various liver conditions including non-alcoholic fatty liver disease and acute liver failure from other causes. Clinical studies suggest NAC may improve insulin sensitivity, reduce inflammatory markers, and support liver function recovery. Typical therapeutic doses range from 600-1800mg daily, though higher doses may be required in acute settings. NAC’s mucolytic properties may cause gastrointestinal side effects, requiring gradual dose escalation and administration with food.
Curcumin Anti-Inflammatory properties in hepatic stellate cell modulation
Curcumin, the primary bioactive component of turmeric (Curcuma longa), demonstrates potent anti-inflammatory and antifibrotic effects relevant to liver disease progression. The compound inhib
its nuclear factor kappa B (NF-κB) signaling pathway, reducing production of pro-inflammatory cytokines including tumor necrosis factor-alpha and interleukin-6. In hepatic stellate cells, curcumin prevents activation and proliferation, key processes in liver fibrosis development.
Preclinical studies demonstrate curcumin’s ability to reduce liver inflammation, prevent fibrosis progression, and support hepatocyte regeneration. However, curcumin’s poor bioavailability presents therapeutic challenges, with standard preparations showing minimal systemic absorption. Enhanced formulations including liposomal curcumin, curcumin phytosome complexes, and piperine combinations significantly improve bioavailability and therapeutic potential. Clinical studies suggest doses of 500-1000mg daily of bioavailable formulations may provide hepatoprotective benefits, though larger randomized trials are needed to establish definitive efficacy.
Alpha-lipoic acid mitochondrial function enhancement protocols
Alpha-lipoic acid (ALA) functions as a unique antioxidant capable of regenerating other antioxidants including vitamin C, vitamin E, and glutathione. The compound demonstrates both water and fat solubility, enabling cellular membrane penetration and mitochondrial protection. ALA particularly benefits liver health through enhancement of mitochondrial function, reduction of oxidative stress, and improvement of insulin sensitivity—all critical factors in hepatic metabolic disorders.
Clinical studies indicate ALA supplementation may improve liver enzyme levels, reduce hepatic steatosis, and enhance insulin sensitivity in patients with non-alcoholic fatty liver disease. The compound also shows promise in diabetic hepatopathy and alcohol-related liver damage. Therapeutic protocols typically employ 300-600mg daily of R-lipoic acid, the naturally occurring and more bioactive form. Some studies utilize higher doses up to 1800mg daily for specific conditions, though gastrointestinal tolerance may limit higher dosing in sensitive individuals.
Mediterranean diet implementation for optimal hepatic health
The Mediterranean dietary pattern provides comprehensive hepatoprotective benefits through its emphasis on anti-inflammatory foods, healthy fats, and nutrient-dense plant foods. This evidence-based nutritional approach demonstrates superior outcomes for liver health compared to conventional low-fat diets, particularly in patients with metabolic liver disease. The diet’s combination of monounsaturated fats, omega-3 fatty acids, polyphenols, and fiber creates synergistic effects that support liver function and reduce disease progression.
Key components of hepatoprotective Mediterranean eating include extra virgin olive oil as the primary fat source, providing oleic acid and phenolic compounds that reduce liver inflammation. Fatty fish consumption 2-3 times weekly supplies omega-3 fatty acids EPA and DHA, which demonstrate anti-inflammatory and antifibrotic properties. Regular consumption of nuts, particularly walnuts and almonds, provides additional healthy fats, vitamin E, and magnesium. Colorful vegetables and fruits supply diverse polyphenols and antioxidants that support hepatic detoxification pathways and protect against oxidative damage.
Whole grains replace refined carbohydrates, providing fiber that supports healthy gut microbiota and reduces hepatic lipogenesis. Legumes offer plant protein, soluble fiber, and resistant starch that promote beneficial metabolic effects. Moderate red wine consumption, traditionally included in Mediterranean patterns, requires careful consideration in liver disease patients, with potential benefits from resveratrol and polyphenols balanced against alcohol-related hepatotoxicity risks. Most hepatologists recommend avoiding alcohol entirely in patients with existing liver disease.
Implementation strategies focus on gradual transitions rather than dramatic dietary overhauls. Starting with olive oil substitution for other cooking fats, increasing vegetable portions, and incorporating fatty fish twice weekly creates sustainable changes. Meal planning approaches emphasize variety, seasonal produce, and traditional Mediterranean preparation methods that preserve nutrient content and enhance palatability. Clinical studies demonstrate that adherence to Mediterranean dietary patterns can reduce hepatic steatosis by 20-30% and improve insulin sensitivity within 6-12 weeks of implementation.
Lifestyle modification strategies for hepatic regeneration and protection
Comprehensive lifestyle interventions provide the foundation for liver health optimization and disease reversal, particularly in early-stage liver conditions. These evidence-based approaches work synergistically with nutritional interventions and medical treatments to maximize hepatoprotective outcomes. The liver’s remarkable regenerative capacity responds favorably to sustained lifestyle modifications, often showing measurable improvements within weeks to months of implementation.
Physical activity protocols specifically designed for liver health emphasize both aerobic exercise and resistance training components. Moderate-intensity aerobic exercise for 150-300 minutes weekly promotes hepatic fat oxidation, improves insulin sensitivity, and reduces systemic inflammation. Activities such as brisk walking, cycling, or swimming provide accessible options for most patients. Resistance training 2-3 times weekly enhances muscle mass, improving glucose metabolism and reducing hepatic glucose production. High-intensity interval training shows particular promise for reducing hepatic steatosis, with studies demonstrating superior fat reduction compared to steady-state cardio.
Sleep optimization plays crucial roles in liver health through regulation of circadian rhythms that control hepatic metabolism. Poor sleep quality and insufficient sleep duration correlate with increased liver enzyme levels, hepatic steatosis, and insulin resistance. Targeting 7-9 hours of quality sleep nightly supports natural liver detoxification processes that occur predominantly during sleep phases. Sleep hygiene protocols include consistent bedtimes, limiting blue light exposure before sleep, maintaining cool sleeping environments, and addressing sleep disorders such as sleep apnea that commonly occur in liver disease patients.
Stress management interventions address the hepatotoxic effects of chronic stress through cortisol dysregulation and inflammatory pathway activation. Chronic stress promotes hepatic lipogenesis, impairs insulin sensitivity, and accelerates liver disease progression. Evidence-based stress reduction techniques include mindfulness meditation, yoga, tai chi, and progressive muscle relaxation. These practices demonstrate measurable reductions in inflammatory markers and improvements in liver enzyme levels when practiced consistently. Workplace stress management requires attention to occupational hepatotoxin exposure, shift work effects on circadian rhythms, and ergonomic factors that influence overall health outcomes.
Environmental toxin reduction strategies focus on minimizing exposure to known hepatotoxic substances in daily life. Common household and occupational exposures include volatile organic compounds, heavy metals, pesticide residues, and industrial chemicals. Practical reduction strategies include choosing organic produce when possible, using natural cleaning products, ensuring adequate ventilation in chemical-exposed environments, and filtering drinking water to remove potential contaminants. Regular detoxification support through sauna therapy, adequate hydration, and supporting natural elimination pathways enhances the liver’s ability to process unavoidable environmental exposures.
Smoking cessation represents a critical intervention for liver health, as tobacco use accelerates liver fibrosis progression and increases hepatocellular carcinoma risk. Nicotine replacement therapy, behavioral counseling, and pharmacological interventions support successful cessation efforts. The liver benefits from smoking cessation become apparent within months, with continued improvements over years of sustained abstinence. Comprehensive cessation programs address both nicotine dependence and behavioral patterns, achieving higher long-term success rates than single-intervention approaches.